This story originally appeared here.
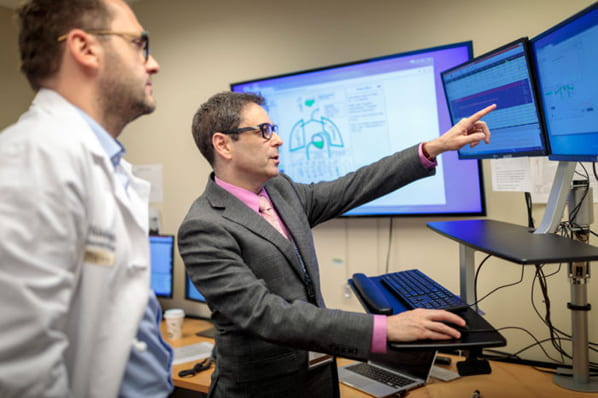
Michael Avidan and his colleagues sit in a windowless room in front of a panel of screens tapped into every operating room at Barnes-Jewish Hospital.
It’s conceptually similar to an air traffic control tower, except they aren’t tracking airplanes. Relying on customized software, the screens provide synthesized data about patients, keeping track of issues such as heart disease, diabetes and emphysema, as well as rapidly changing physiological measurements including blood pressure, heart rate, temperature, the brain’s electrical activity and other vital signs that anesthesiologists monitor during surgeries. Avidan and the others closely watch the data as part of a study examining whether such oversight can help provide better outcomes for patients.
Avidan, an anesthesiologist at Washington University School of Medicine in St. Louis, zeroes in on one of the patients. “We can see where there potentially could be issues here,” said Avidan, MBBCh, the Dr. Seymour and Rose T. Brown Professor of Anesthesiology. “Based on everything we know about this patient, and concerning data that’s streaming live from the operating room, I worry about this patient’s risk for developing renal failure.”
Each day, a team of anesthesiologists, anesthesiology residents, and nurse and student-nurse anesthetists work together in the so-called Anesthesiology Control Tower to identify potential risks to patients and consider what measures might be taken to optimize those patients’ perioperative outcomes. As part of the study, they communicate with the clinicians in half of the operating rooms every day, making suggestions when deemed helpful.

For the other half of the operating rooms, control tower clinicians monitor what’s happening and note potential problems in a computer log. But they don’t intervene unless there is a threat to patient safety and well-being. The study, called ACTFAST, also includes other researchers from the Department of Anesthesiology and from the Department of Surgery.
“Ultimately, we want to know if the Anesthesiology Control Tower complements the care provided by clinicians on the ground,” Avidan explained. “Our overarching goal is to enhance the quality of perioperative care and to contribute meaningfully to patient safety and outcomes.”
Another important goal of the project is to develop computer algorithms that may be able to identify patterns suggesting that patients are at risk for specific complications — such as heart attack, respiratory failure or death. Such forecasting algorithms could assist physicians in the control tower as they monitor operations. That aspect of the ACTFAST study involves colleagues from the Department of Computer Science & Engineering, as well as anesthesiology.
Separate but unequal
Avidan first started designing studies and doing research during his residency in South Africa, where he was born and studied medicine.
“I was asking a lot of questions,” recalled Avidan, who also is a professor of surgery. “But I had no real research training and was trying to figure out how to put studies together, work with an institutional review board and do the other things required to conduct good research, but it was difficult to feel my way through. So I thought, ‘I need to get some academic training.’”
Growing up in South Africa, Avidan chose health care as a career because he wanted to do something that would satisfy him intellectually while allowing him to contribute to a society that was unequal and divided, due largely to apartheid, a system of racial segregation and white supremacy.
During his training, Avidan worked in hospitals in urban and rural areas, serving at Chris Hani Baragwanath Hospital in Soweto and at Tintswalo Hospital in rural Gazankulu.
“The professed philosophy underpinning apartheid was that different racial groups should be kept separate, but equal,” he said. “Apartheid literally means separateness, and this was successfully enforced. But equality never was truly the goal, and disparity was built into the fabric of the society.”
That was true in all areas of life, including health care.
“There were hospitals that were only for white people and hospitals that were only for black South Africans,” he said. “The hospitals for white people had wonderful resources and would compare favorably, in terms of technology, with any hospitals in the world. But the hospitals that served black communities, such as Baragwanath, were understaffed, overcrowded and very poorly resourced. When I was a student, several of us said we would only work in the hospitals with fewer resources until this segregation in health care was done away with and anyone could receive health care in any hospital.”
He recalled treating large numbers of knife and gunshot injuries while working in Baragwanath Hospital, which is on the outskirts of Soweto, a sprawling ghetto that is a township of the city of Johannesburg. He also remembered that the hospital had only two operating rooms where cesarean sections were performed, and both were booked all day and night, with no breaks. Later, while a junior doctor working weekends at rural Tintswalo Hospital, Avidan was one of only two physicians on site to cover all 500 hospital beds.
Training in the UK and USA
After completing his training in anesthesiology and intensive care medicine in South Africa, Avidan decided to advance his academic career in London, where he became a clinical lecturer at King’s College Hospital.
Avidan obtained advanced training in clinical research, as well as in cardiac anesthesiology and critical care medicine. In 2001, he accepted a position as a visiting professor at Washington University, intending to spend about a year enhancing his research skills, but “the best laid plans of mice and men are seldom realized,” he said.
With the exception of a one-year stint back in England, he’s been here ever since.
“I was impressed by what I experienced at Wash U,” he said. “In the U.K., when I wanted to study things that were a bit different, many people would discourage me and tell me not to rock the boat. But here, Alex Evers — the head of anesthesiology — and others would say, ‘Sure. How can we help you?’”
Since his arrival at Washington University, Avidan has studied, among other things, the phenomenon of intraoperative awareness, when patients report remembering often distressing things that happened while they were undergoing surgery while under general anesthesia. He also led an international study of the drug ketamine, frequently given to patients with the aim of reducing postoperative pain and confusion following surgery. His international team, however, found the drug didn’t lower pain levels and that it made older patients more likely to have hallucinations and nightmares after surgery.
Now, he’s leading an effort to use telemedicine, artificial intelligence and machine learning to improve outcomes for surgical patients. This is why he sits in front of those screens in that windowless room, learning what happens when other sets of eyes — and computers that may recognize patterns people don’t — monitor patients to keep them safer during surgery.
“You can imagine that in the future we may be able to offer these resources to somebody in, say, rural Missouri, where they may not have as much expertise and experience with certain operations,” he said. “They could call on us, and we could monitor things, and as we advance in artificial intelligence and machine learning, we may develop a whole arsenal of tools to make perioperative care more efficient and contribute to improving patient outcomes.”
But first, they have to prove whether patients really do better with such an approach. The new study is one reason he remains so excited about working at Washington University a decade and a half after he first arrived here.
But he admits that stimulating research projects aren’t the only reason he stayed.
“My wife, Tracey, is from St. Louis,” he said. “I met her in a rock-climbing gym, and we hit it off. We both like the outdoors. For our honeymoon, we went rock climbing near Yosemite. We’ve even been rock climbing back in South Africa. We traveled extensively before we had kids.”
Their daughter, Naomi Hannah, is 6, and their son, Alon Joseph, is 4. The couple does less rock climbing these days, but Avidan still travels across the Atlantic to visit the rest of his family and meet with fellow members of the editorial board of the British Journal of Anesthesia.
And on those flights across the ocean, Avidan is particularly mindful of the air traffic controllers paying heed to the crisscrossing airplanes, much as in the Anesthesiology Control Tower at Barnes-Jewish Hospital, where he and his colleagues attend to surgical patients in multiple operating rooms.
