The Well-being Word

Associate Vice-Chair of Well-Being
Hi friends — Happy New Year!
A new year often invites reflection and change, both personally and professionally. Change can be exciting and uncomfortable at the same time.
Adapting to change does not mean forcing positivity or pretending that transitions are always easy—because they certainly are not (I know; I personally have made 42,000 wrong turns in the new building, and don’t even get me started on the walls that pop up over the weekend, changing a route you have walked for a decade)! Turning change into a positive experience means acknowledging that uncertainty can feel uncomfortable while ALSO recognizing that growth often lives in that discomfort. Research consistently shows that people who can reframe change as an opportunity for learning and connection experience less burnout and greater job satisfaction over time. Adaptation is not passive—it is an active skill we all need to practice.
Giving ourselves permission to feel uncertainty, approach things with curiosity, ask for support, and redefine success during transitions protects both confidence and well-being. Strong teams are built when we intentionally welcome change and remain open to different ways of thinking and doing. Many of the changes that will occur this year will quietly shape our daily experience. It is up to us to create this new normal.
As we navigate all of this, take a moment to reflect on what you love about working here. Is it the people who support you on hard days? The commitment to excellence and learning? The opportunity to teach, mentor, and grow? The sense of purpose that comes from caring for patients and families during vulnerable moments? Or the pride of being part of a department that continues to evolve and lead?
Remembering what you love about where you work is not nostalgia. You are not “stuck in the old days.” It reminds us why adapting is worth the effort. When our “why” is clear, change becomes something we move through together, not something that happens to us.
There is a lot of science and research behind managing and adapting to change! Read below for a little more education on how we all process and move through change. And be sure to check out the Well-developed Podcast episode #20 on Change Management with Angie Clark.
Cheers to a new year, new change, and a commitment to continued success and growth!
What’s ahead?
- Dec. 15 – Jan. 16 | Holiday Lights Recycling
- Jan. 19-23 | MLK Commemoration Week
- Jan. 29 | Installation of Anne M. Drewry, MD as the Llorin-Roa Professor of Anesthesiology
- Feb. 19-24 | Lab Supply Swap – WashU labs are invited to donate surplus lab supplies and equipment and/or acquire needed lab materials for free.
- April 11 | Supporting Women of WUDA retreat (more information to come soon!)
- May 26 | C.R. Stephen Lecture featuring Max B. Kelz, MD, PhD (more information to come soon!)
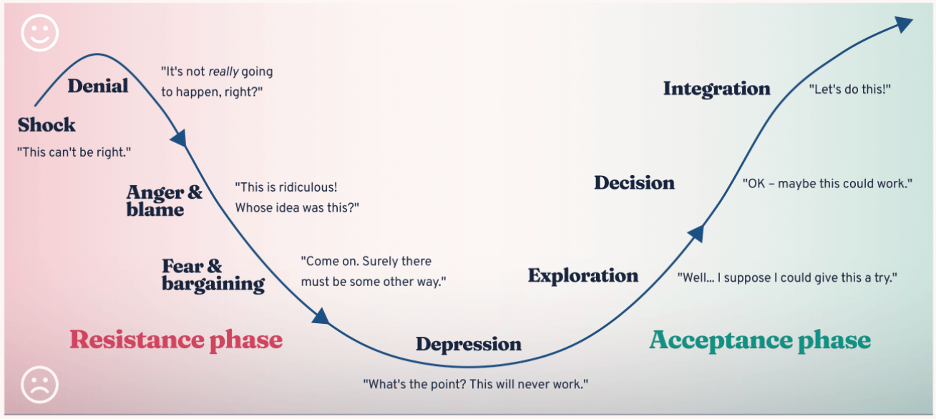
Kübler-Ross Change Curve
Originally developed to describe grief, the Kübler-Ross Change Curve has since been widely used to describe how people experience and process change of all kinds.
Change rarely arrives quietly and smoothly. It often shows up as disruption, uncertainty, or even anger and fear. The curve offers a framework for understanding why those reactions are so common, and so normal.
The curve shows us that change is not a single moment, but a journey. Early stages of change may include shock, frustration, or resistance, when things feel harder than expected. Over time, many people move through periods of confusion or self-doubt before gradually reaching acceptance, adaptation, and engagement.
As you navigate change, this curve can serve as a checkpoint.
Pause and ask yourself: Where might I be on the curve right now? Naming your place on the curve can help you process and gain some self-awareness. And hopefully some motivation to keep going!
With time, reflection, adjustment, and support, people do reach the other side (even if you hit a few bumps and backslides along the way). New routines and new ways take hold. If you are in a difficult phase right now, remember: this is part of the process, and it will get better.
A Day in the Life of Diana Prichard, CRNA

As Chief CRNA, Diana plays a key leadership role in ensuring the day runs smoothly for both patients and providers in West County. Her work extends beyond the operating room, encompassing leadership, coordination, and support for a multidisciplinary team in a fast-paced clinical environment. In this “Day in the Life,” Diana offers a behind-the-scenes look at what it takes to lead with intention, adaptability, and a strong commitment to team-based care.
An anesthesia day has a rhythm we all know—early mornings, precise work, and teamwork that becomes second nature. As Chief CRNA, my role is to support a team that already works well together; along with coordinating scheduling, staffing, and working through unexpected challenges so that patient care runs at the highest level. The compassion and skill our CRNAs, physicians, nurses, and technicians bring to each day make all the difference, and I’m honored to be part of it.
5:30 a.m.—My day begins by reviewing the schedule, checking emails and text messages, and noting any overnight updates. Early preparation allows the team to anticipate challenges and stay on track.
6:00 a.m.—Sick callouts and last-minute changes are addressed quickly. Cases are reassigned, coverage is confirmed, and workloads are balanced to keep the day running efficiently. The anesthesia assignment board is completed and sent out to all of the CRNA’s so everyone is on the same page for the day.
6:30 a.m.—Our Lead Anesthesia Tech (Kim), Associate Chief (Emily), and OR Charge Nurse all check in with each other to review the schedule, discuss add-ons, and identify potential workflow or equipment issues. Collaborating early ensures there is a strong start to the day.
6:45–7:15 a.m.—Set up for my cases of the day. If anyone is running late or has questions we are there to help.
7:15–8:00 a.m.—Cases begin across three locations—the Orthopedic Center (5 ORs), the ASC (4 ORs), and Barnes West County Hospital (14 ORs, 5 Endo rooms, and an IR/CT suite). Between cases, my team and I together help troubleshoot IT issues, resolve workflow questions, and support new CRNAs as they navigate protocols and workflows, and our seasoned CRNA’s should any issues arise.

8:00–12:00 p.m.—Clinical time! The department runs smoothly with quick turn over times, and staff take care of each other by offering breaks/helping with other cases if there is downtime.
12:00–2:00 p.m.—Continued clinical time, but I also help make sure staff are getting lunch breaks, review the rest of the weeks schedule, anticipate staffing challenges, and make proactive adjustments. As rooms start to come down for the day, I work closely with the OR Charge to move cases and staffing around as needed and help make decisions about relief if there are questions. Planning ahead keeps patient care and our staff supported.
2:00 p.m. – Time to review emails, talk with Emily to make sure we follow up on any outstanding requests, create and disburse any education and attend meetings as needed. This behind-the-scenes work ensures the department operates effectively and that staff concerns are addressed and everyone is kept up-to-date with important information.
3:00–5:30 p.m. – The team and I continue our focus on patient care and helping with the board and relieving staff.
5:30–7:00 p.m. – As the last cases finish and our patients are safely in recovery, I meet with staff as needed and confirm coverage for the next day. Operational issues are reviewed, and adjustments are made. When the day winds down, I head home, knowing tomorrow will bring another set of challenges and opportunities to support our team.
While many of my days begin in the OR, the rhythm of my life is shaped just as much by what happens outside of it. Travel has become one of the ways I reset and return to work with renewed clarity. Even on a normal morning, I often think back to recent adventures—like wandering the serene temples of Kyoto, walking through the crowded streets of Tokyo, or taking in the breathtaking stillness of Mt. Fuji. (In case you couldn’t tell I just got back from Japan… and yes, you absolutely should go!)







The best part of my days are the time I get to spend with my family. Their love and support keep me grounded and remind me of what truly matters. Most evenings you can find us sharing a meal together, talking about our days, or getting out to cheer on the kids—whether it’s watching my 15-year-old son, Cade, race at his cross-country meets (10th grade at Whitfield), or supporting my 13-year-old daughter, Evie, at her volleyball games (8th grade at Whitfield). Through it all, my husband of 20 years, Wayne, remains a constant source of strength and inspiration for me.



Some days are busier than others—whether I’m in the OR, out seeing the world, or juggling life at home—but each setting gives me something essential. The intensity of the OR sharpens my purpose, travel broadens my perspective, and the quiet moments at home help me recharge, always reminding me that connection is what truly sustains me—both in my personal life and within my team at work.






PIA SAFE Corner
This month, we’re focusing on how to support colleagues after adverse events and during debriefs. These conversations can be uncomfortable, emotional, and hard to navigate.
Key ways to support a colleague
- Normalize, don’t minimize: “It makes sense to feel this way.”
- Reassure purpose: “This is about learning, not blame.”
- Reflect feelings: “I hear how heavy this feels.”
- Offer choice: “Would you like to step out or talk later?”
Watch for signs of distress
Withdrawal, tearfulness, anger, excessive self-blame, or difficulty concentrating. If present, pause and check in privately.
After the debrief
Follow up, share support resources, and remind them: “I’m here when you’re ready.”
PIA SAFE is a peer-based program in the Department of Anesthesiology designed to address concerns about negative behaviors, conflicts, and microaggressions experienced by department members. Check out the PIA SAFE website or email Erin Herrera (erinherrera@wustl.edu) to learn more!

The Well-developed Podcast – 3 New Episodes for 2026!
We just released three new episodes diving into career pivots, wellness, and physical therapy.
If you’ve read this far in this month’s newsletter—thank you! The first five people to email me (erinherrera@wustl.edu) will receive a digital Starbucks gift card — thank you for supporting the Health & Wellness Newsletter!
When you’re not at your best, it’s hard to learn or perform well. The Well-developed Podcast offers a space to reflect, recharge, and explore how bringing your whole self to work can boost your personal and professional growth. Discover how your unique strengths, values, and preferences can support your well-being and development.
Have an idea for a podcast topic? Share your suggestions using the form at the bottom of our webpage. Thanks for influencing our podcast’s evolution!

Take 2 for the Team
This quick and easy platform encourages everyone in the department to take just two minutes out of their day to send a note of appreciation to a colleague. Accessible via the departmental INTRAnet, the app delivers your message of thanks straight to your teammate’s inbox.
Take a moment today to celebrate the people who help make our department a better place to work. A small gesture can go a long way.