The Well-being Word
Why Quality & Safety Matter for Our Well-being

Associate Vice-Chair of Well-Being
Hi Friends,
Here’s a little secret: Well-being doesn’t live in a silo. Some of my greatest allies in this work might surprise you. One of the biggest? The Safety & Quality team! They may not be the first group you think of when it comes to well-being, but trust me — their work is a game changer. Want to know why? Let’s break it down!
We spend so much of our time and energy focused on providing the best possible care for our patients. The mental effort required to juggle all the tasks, decisions & information involved in patient care is a LOT.
That information overload is called cognitive load, and as clinicians in modern healthcare, we all carry a heavy cognitive load.
As clinicians, we put a ton of pressure on ourselves: to know it all, to stay current on every new guideline, to be thorough and perfect, and to give every patient the best care possible.
That’s noble, but it’s also exhausting and not sustainable.
When our cognitive load becomes too heavy, it not only wears us down but also affects our practice and interactions with patients and teams. We are at higher risk of burnout, increased medical errors, less time at the bedside with patients, lower job satisfaction, and a higher chance of negative behavior and team interactions.
A cluttered, overloaded brain makes our work harder and less rewarding.
The good news? We can do something about it! A significant aspect of quality improvement is reducing cognitive load, allowing us to focus on what matters most — caring for patients.
Lots of work is already happening behind the scenes in our department to help us all work smarter, not harder, and be the best clinicians possible.
- Evidence-based Protocols, Guidelines & Checklists — Protocols, smart phrases, order sets, and checklists create standard work that builds reliability, consistency, and safety into daily practice.
- Epic Alerts — Don’t forget that blood glucose and Ancef redose! The allergy bar is yellow! Technology helps us catch potential issues before they catch us.
- CPAP Assessments — CPAP saves us so much time and cognitive load by sorting through entire charts for us. Consolidating patient information in an organized, consistent way ensures that important information does not get overlooked at critical times.
- MPOG Data — Learning from patterns to improve outcomes and processes help us easily identify areas to focus on for personal improvement as well as trends across our divisions
- Workflow Improvements — Turnover “showtimes” are just as much about getting YOU out on time as it is getting cases done. When we all work more efficiently in our workspaces, we can spend more time with patients and give more thorough, attentive, and personalized care.
- Safety Event and Near Miss Identification & Learning — Curating informative, judgment-free M & M’s helps us learn to all be better and creates a culture where learning from systems issues help us all improve.
When we reduce cognitive load and foster a psychologically safe and learning culture, we don’t just create smoother days, we create better patient care, which fuels our pride and meaning in our work and improves our professional fulfillment, all of which are key drivers in our workplace well-being.
Engaging in QI projects empowers you to positively impact the work and culture that shapes your day-to-day. Not just for yourself, but for everyone. Quality improvement and patient safety don’t just protect our patients; they also protect us. Taking on a QI project might not only improve patient care… it could improve your own well-being too.
The center for INformatics, QUality Improvement, REsearch, & Safety (INQUIRES) team sent out a great newsletter in September. Be sure to check out all the great things coming out of their office and ways to get involved.
What’s ahead?
- Sept. 15 – Oct. 15 | Latine/Hispanic Heritage Month
- October 7 | Disability Employment Awareness Panel Discussion
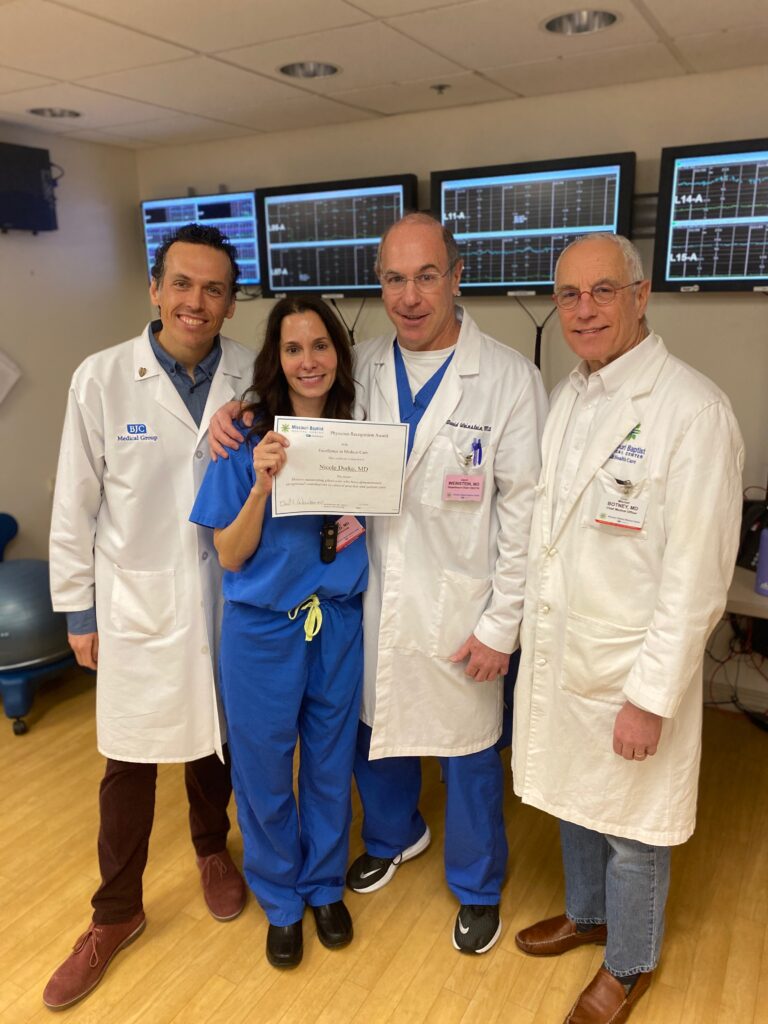
A Day in the Life of Nicole Durko, MD

This month’s Day in the Life takes you inside a day of Nicole Durko, MD, Associate Chief of the Division of Obstetric Anesthesiology at WashU Medicine. From leading patient care at Missouri Baptist Hospital to cheering on her son’s hockey team, Nicole balances a demanding career with family life, fitness, and plenty of St. Louis adventures.
WORKDAY
4:30 a.m. – Wake up, grab breakfast (always with a Diet Coke), and review the patient board before I even step into the shower. This helps me start the day already knowing who I’ll be caring for.
5:00–6:00 a.m. – Shower, tidy up the house, and make sure everything is ready for my kids’ school day since I’ll be away for 24 hours.
6:30 a.m. – Arrive at the hospital. We do change-of-shift with the anesthesiologist and two CRNAs coming off the night shift. After handoff, the day takes off quickly.
Morning–Afternoon – The hours are filled with labor epidurals and C-sections. Our service is busy and fast-paced but incredibly rewarding. Alongside clinical care, I’m often juggling administrative responsibilities: patient consultations, pharmacy discrepancies, supply chain issues, and meetings that keep our OB anesthesia service running smoothly.

3:00 p.m. – I try to give my CRNAs a break around this time and personally cover most of the cases. It’s important to me to support the team and ensure everyone gets a moment to breathe during a long day.
Evening–Overnight – The pace never really slows down. OB is a 24/7 specialty, and the calls can come at any hour. By the time morning rolls around, I’ve usually been through a mix of deliveries, emergencies, and late-night consultations.
Non-Workday

6:30 a.m. – Wake up and start the day by taking my daughter, Nina, a 10th grader at Villa Duchesne, to school.
7:30 a.m. – Head to Shred415, my “home away from home,” where I love to work out and have made many friends.
Late Morning – Usually a quick stop at the grocery store, then grabbing a salad at Sportsman’s Park between meetings.
Afternoon – With the house quiet, I usually return to administrative tasks at my computer and catch up on projects. On some days, I even have free time to volunteer at my kids’ schools—working in the Villa Boutique at Nina’s school or serving lunch at Drake’s school, Chaminade.
Afternoon–Evening – Family time is the priority. Nina (15) keeps me busy with homework and field hockey, while Drake (17), a junior at Chaminade College Preparatory School, has a packed hockey schedule. Thankfully, since he drives himself, that part is a little easier.
Night – I wind down by spending time with my family, knowing another busy workday is always just around the corner.





PIA SAFE
September was National Suicide Prevention Month and we wanted to share some warning signs of distress and how to safely support friends, family, and colleagues.
- The AAMC has an excellent script for approaching a distressed colleague. Please keep this handy.
- Crisis resources: You can call 988 or text TALK to 741741 — available 24/7.
- WashU Support: WashU Psychiatry offers expedited care for employees and their families.
PIA SAFE is a peer-based program in the Department of Anesthesiology designed to address concerns about negative behaviors, conflicts, and microaggressions experienced by department members. Check out the PIA SAFE website or email Erin Herrera (erinherrera@wustl.edu) to learn more!

The Well-developed Podcast — Six new episodes!
In July 2025, we release six fresh episodes diving into hobbies, coaching, trust, growth, conflict, and change.
When you’re not at your best, it’s hard to learn or perform well. The Well-developed Podcast offers a space to reflect, recharge, and explore how bringing your whole self to work can boost your personal and professional growth. Discover how your unique strengths, values, and preferences can support your well-being and development.
Have an idea for a podcast topic? Share your suggestions using the form at the bottom of our webpage. Thanks for influencing our podcast’s evolution!

Take 2 for the Team — Update!
Our peer-to-peer gratitude app, Take 2 for the Team, just got even better! The latest update adds all of our amazing anesthesia techs to the dropdown menu—making it easier than ever to recognize and thank them for their vital contributions.
This quick and easy platform encourages everyone in the department to take just two minutes out of their day to send a note of appreciation to a colleague. Accessible via the departmental INTRAnet, the app delivers your message of thanks straight to your teammate’s inbox.
Take a moment today to celebrate the people who help make our department a better place to work. A small gesture can go a long way.

WUDA Supporting Parents Group
This program not only aims to foster a supportive and connected community for parents within our department, but also serves as a tool for others so they can stay up to date on key WashU/BJC benefits, policies, and more.
This group is dedicated to creating a resource hub and community where parents feel informed, empowered, and connected throughout their parenthood journey. We aim to provide easy access to information on all aspects of parenthood and to connect parents within our department.