A new study published in JCI Insight suggests that interleukin-7 (IL-7), a key immune-boosting cytokine, may help critically ill COVID-19 patients by reducing life-threatening secondary infections. Led by Richard S. Hotchkiss, MD, professor of anesthesiology, medicine, surgery, and developmental biology at WashU Medicine, the study highlights IL-7’s ability to enhance immune recovery without triggering harmful inflammation.
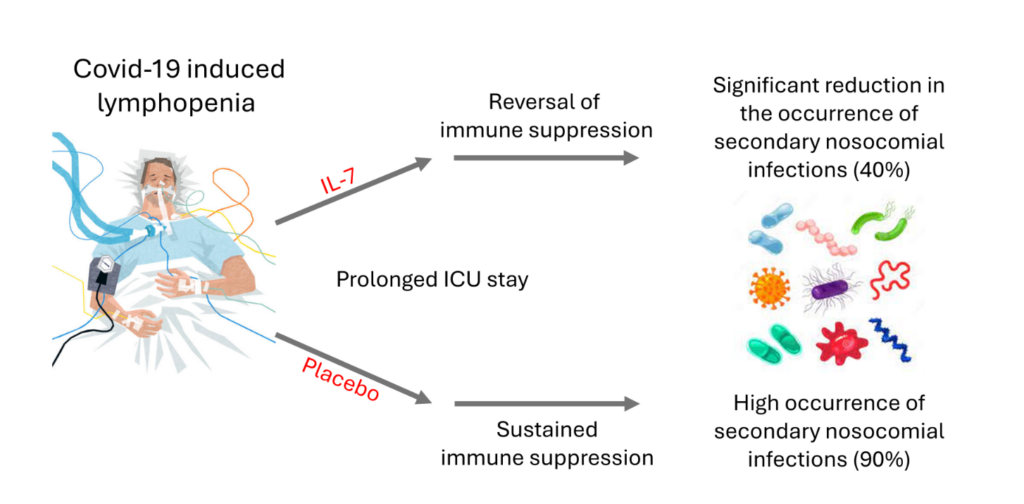
COVID-19 often leads to lymphopenia, a dangerous depletion of lymphocytes which are key immune cells responsible for fighting infections. Patients with low lymphocyte levels are more vulnerable to prolonged illness and hospital-acquired infections—a major cause of COVID-related deaths.
“Unlike many immune therapies used in COVID-19 that acted to suppress inflammation, IL-7 is unique—it enhances the immune response by boosting CD4 helper and CD8 cytotoxic T cells, which are essential for viral elimination and immune recovery,” said Hotchkiss. “This makes IL-7 a promising candidate for improving outcomes in immunocompromised COVID-19 patients.”
The randomized, placebo-controlled trial included 109 critically ill, lymphopenic COVID-19 patients to evaluate the effects of CYT107, a recombinant IL-7 therapy. The study’s key findings include:
- Fewer hospital-acquired infections: Patients who received IL-7 had 44 percent fewer secondary infections than those receiving a placebo. This is particularly significant since secondary infections are a major cause of death in hospitalized COVID-19 patients.
- Potential to reduce ICU and hospital stays: IL-7-treated patients showed strong trends toward shorter ICU and hospital stays compared to the placebo group.
- Safety and tolerability: CYT107 was safe and well-tolerated, with no evidence of cytokine storm or worsening lung function. Additionally, patients receiving IL-7 experienced fewer treatment-related adverse events than those in the placebo group.
- Lymphocyte recovery: While both groups experienced an increase in lymphocyte counts, patients who received IL-7 without antiviral therapy, which can suppress lymphocyte levels, had a 43 percent increase in final lymphocyte count than the placebo group.
“Given that hospital-acquired infections significantly contribute to COVID-19 deaths, IL-7’s ability to lower infection rates could lead to better survival outcomes,” the authors wrote.
Researchers believe IL-7 could have applications beyond COVID-19, particularly in severe respiratory viral infections where immune suppression increases mortality. However, further clinical trials are needed to explore IL-7’s full potential in different patient populations.
For more details, read the full study in JCI Insight.